Every January, as the festive season winds down and the chilling winter sets in, you might notice a familiar, unwelcome sensation: intensely itchy and scaly lower legs. This annual ritual of discomfort can turn a cozy winter evening into a frustrating ordeal. But why does this happen, and what can you do when your doctor is unavailable?
Understanding the root causes of your itchy legs and knowing how to manage them effectively can bring much-needed relief. In this article, we will explore why your lower legs become especially prone to dryness and itchiness during winter, and provide practical solutions you can implement today to soothe your skin and restore comfort.
1. Why Your Lower Legs Freak Out Every January
The winter months bring a drop in humidity levels, both outdoors and indoors, as heating systems dry out the air. Your skin, particularly on your lower legs, can lose moisture rapidly in these conditions, leading to dryness and irritation. The skin on your legs is naturally thinner and has fewer oil glands than other parts of your body, which makes it more susceptible to dryness.
Moreover, the cold weather often prompts us to take longer, hotter showers, which can strip the skin of its natural oils. This exacerbates the problem, as without its natural barrier, the skin becomes even more prone to becoming dry, itchy, and scaly. These factors combined create the perfect storm for winter itchiness, particularly on the lower legs.
2. How To Tell If It Might Be Asteatotic Eczema (a.k.a. Winter Itch)
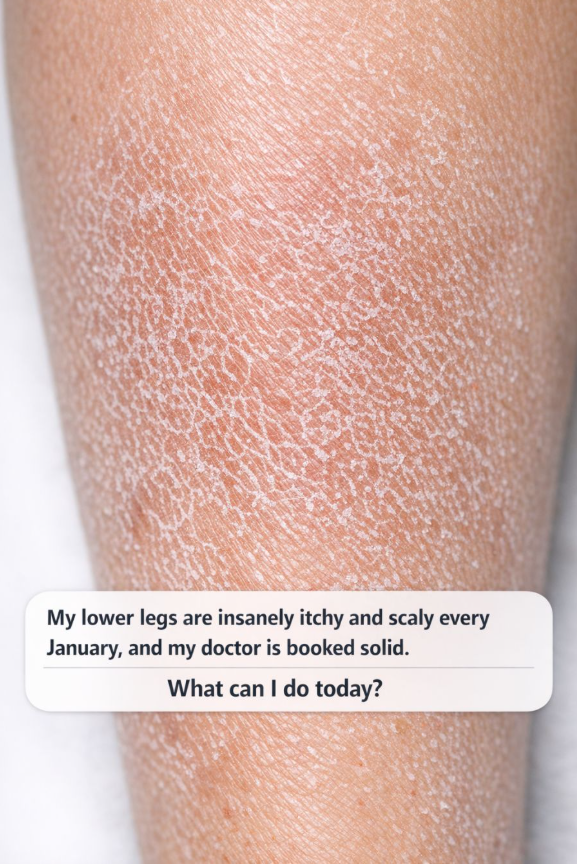
Asteatotic eczema, commonly known as winter itch, is characterized by dry, cracked, and itchy skin, often appearing on the lower legs. It can look like a network of fine cracks over the skin, which may resemble a dry riverbed. If you notice your skin is not only dry but also has a red, irritated appearance with these fine cracks, it might be more than just typical dryness.
Pay attention to any accompanying symptoms like slight swelling or a burning sensation. Asteatotic eczema can be distinguished from regular dry skin by these additional discomforts and its persistence despite regular moisturizing.
3. The Immediate “Do No Harm” Rule: Stop These Common Irritants Today
One of the first steps in managing itchy, scaly skin is to eliminate potential irritants from your routine. This includes avoiding harsh soaps and detergents which can strip the skin of essential oils. Opt for mild, fragrance-free cleansers instead.
Also, be mindful of your clothing choices. Wool and synthetic fibers can irritate the skin; instead, choose soft, breathable fabrics like cotton. By making these changes, you can prevent further irritation and give your skin a chance to heal.
4. Switch To A Short, Lukewarm, Fragrance-Free Shower Routine Tonight
Long, hot showers may feel wonderful in the cold months, but they can worsen dry skin by removing protective oils. Instead, opt for shorter showers with lukewarm water. Aim for showers that last no more than 10 minutes.
Use a gentle, fragrance-free cleanser to avoid aggravating sensitive skin. Pat your skin dry with a towel after showering instead of rubbing it, which can irritate the skin further.
5. The 3-Minute Rule: Lock In Moisture Right After You Towel Off
To maximize moisture retention, apply a heavy-duty moisturizer within three minutes of drying off after your shower. This three-minute window is crucial because it helps seal in hydration while your skin is still damp.
Choose a moisturizer that is rich in emollients and humectants. Ingredients like glycerin, hyaluronic acid, and ceramides are effective at drawing moisture into the skin and strengthening its barrier.
6. Thick, Greasy, and Boring: The Kind of Moisturizer That Actually Works
For dry, itchy legs, thick, greasy moisturizers like petroleum jelly or ointments are often the most effective. While they may not feel luxurious, they form a protective layer over the skin that locks in moisture and provides relief.
Look for products that are labeled as ‘fragrance-free’ and ‘for sensitive skin’, which are less likely to cause irritation. Apply these moisturizers liberally and frequently, especially after bathing and before bed.
7. Strategic Use of OTC Hydrocortisone: When and How To Try It Safely
Over-the-counter hydrocortisone cream can help reduce inflammation and itchiness associated with winter skin flare-ups. Apply a thin layer to the affected areas once or twice a day, but it’s important not to overuse it.
Limit use to a week at a time and consult with a healthcare provider if symptoms persist. Overuse of steroid creams can lead to skin thinning and other side effects, so careful application is key.
8. Viral TikTok Hacks for Itchy Skin: What Helps and What to Skip
The internet is full of DIY skincare hacks, but not all of them are beneficial. For example, while oatmeal baths can soothe itchy skin due to its anti-inflammatory properties, using lemon juice or baking soda can disrupt your skin’s pH balance and cause further irritation.
Before trying viral hacks, consider their ingredients and potential effects on your skin. Stick to dermatologist-recommended treatments when in doubt.
9. Easy Clothing and Laundry Tweaks That Calm Angry Winter Skin
Switching to soft, breathable fabrics like cotton can prevent further irritation to your skin. Avoid tight-fitting clothes that might rub against your skin and exacerbate dryness.
In the laundry room, opt for hypoallergenic detergents free from dyes and fragrances. Ensure that your clothes are thoroughly rinsed to remove all detergent residue, which can irritate the skin.
10. Humidify Your Space: Simple Home Fixes That Make a Big Difference
Investing in a humidifier can increase the moisture level in your home during the dry winter months. Aim to keep indoor humidity levels between 30-50% to help maintain your skin’s hydration.
Place humidifiers in the rooms where you spend the most time, such as the bedroom and living area. Regularly clean and maintain your humidifier to prevent mold and bacteria growth.
11. When Itching Isn’t “Just Dry Skin”: Red Flags You Shouldn’t Ignore
Persistent itching that doesn’t improve with over-the-counter treatments may signal more serious conditions like psoriasis, fungal infections, or systemic issues like liver disease. If you notice open sores, significant swelling, or changes in skin color, it’s important to seek medical advice.
Other red flags include severe discomfort disrupting your daily activities or sleep, and any accompanying symptoms like fever or weight loss. These could indicate an underlying medical condition that needs attention.
12. How To Document Your Symptoms So Your Doctor Visit (When You Get One) Counts
When you finally get an appointment, having a detailed record of your symptoms can make your visit more productive. Keep a journal noting when your symptoms started, any patterns you notice, and what treatments you have tried.
Include photos of the affected areas to show any changes over time. Note any other health changes or medications that might be relevant. This documentation will help your doctor diagnose the issue more accurately and tailor a treatment plan that suits your needs.